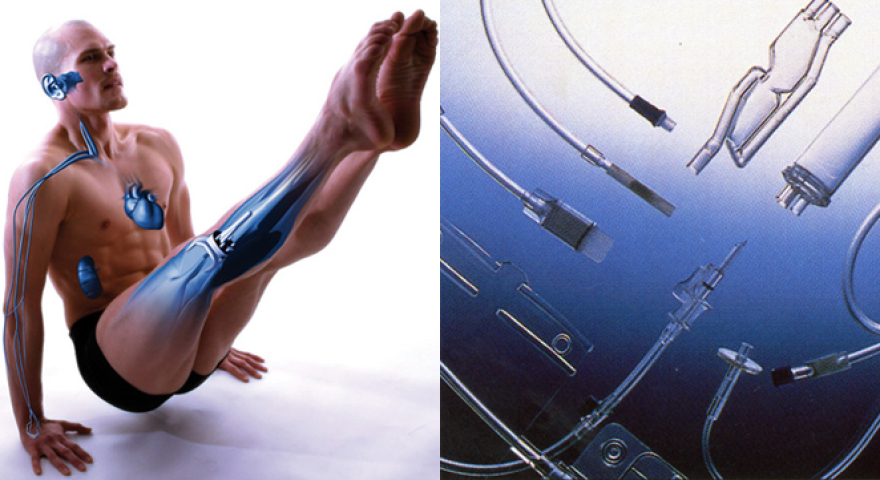
Design for living with absorbable polymers
Medicine may be the one area where biodegradable plastics are most valuable. Bio-absorbable polymers are now used for temporary orthopaedic implants or in slow-release drugs because they soften gradually, slowly lose their resistance and are eventually absorbed into the body.
The plastics in me
For health purposes we regularly ingest many polymers used by drugs manufacturers to regulate the intake of medication. Tablets and capsules may have a superthin biodegradable plastic film coating which serves a threefold purpose. For some drugs, it helps mask an unpleasant taste or smell (the bitter taste of paracetamol, for example).
Then, too, it provides health professionals with a better identifier. Finally, it can help protect the active ingredient of the drug and regulate its dispersion in the body. While natural materials are still used as coatings, polymers are the only game in town for slow-release drugs requiring controlled drug release over time or targeted release for a specific organ. Such is the case, for example, with gastro-resistant drugs that do not disintegrate in the stomach but release their contents further down the line in the intestine.

Microscopic-scale plastics take giant steps forwards
 Some plastics are now essential for targeted drug action; they have enabled novel cyclodextrin-based drug delivery systems derived from starch or biodegradable polymers.
Some plastics are now essential for targeted drug action; they have enabled novel cyclodextrin-based drug delivery systems derived from starch or biodegradable polymers.
They take the form of nanospheres, where the polymer is hyperbranched into networks or nanocapsules where it forms the wall of the compartment containing the lipophilic or aqueous drug.
These nanocapsules navigate for longer in the bloodstream ensuring more controlled release of the therapeutics.
The active ingredients are not dispersed but released at the right point without having previously degraded. Their very low dosage reduces the side effects for patients. Furthermore, nanocapsules provide effective camouflage, slipping under the body’s radar, which changes its immune response to the drug as less harmful.
Dressed to heal
 Ouch, that smarts! The end of tedious wound dressing replacement sessions may be nigh...Before long, we may be dressing the wound, tackling infection and promoting healing in one stroke.
Ouch, that smarts! The end of tedious wound dressing replacement sessions may be nigh...Before long, we may be dressing the wound, tackling infection and promoting healing in one stroke.
Dressings incorporating healing accelerators in the form of an encapsulated active ingredient already exist. The microcapsules are implanted on the foam pad using a polymer-based binder (acrylic, polyurethane, silicone, etc.).
This technique enables the active ingredient to be kept on the pad and speeds the patient’s recovery.
Faster healing through plastic
Researchers have recently developed polymer-based self-healing dressings. The patient’s skin cells are laboratory cultured before being implanted on a polymer membrane to which they adhere before dividing.
They are then applied to the wound and migrate inside it to reproduce and then heal the open wound. This revolutionary technology which eliminates the risk of rejection by the body is already used for diabetic ulcers and burn patients.
Clinical trials are running to extend it to all long-healing wounds. Ultimately, it should ease patient-care by enabling them to be treated at home.

Synthetic sutures - stitch in time !
 Once upon a time, having stitches removed meant a return trip to hospital. Not any more!
Once upon a time, having stitches removed meant a return trip to hospital. Not any more!
Sutures made from polymers like polylactic acid (PLA) (lien interne) or polyglycolic acid are now completely self-dissolving. These absorbable synthetic polymers also exhibit consistent characteristics unlike natural suture materials which may cause unpredictable tissue reactions.
Better yet, polymer threads do not cause secondary inflammation and do promote wound healing.
Bioactive bone implants
 The same principle applies to the polymer composites for bone replacement or temporary implants. For many years, broken bones have been mended with metal implants or replaced with bone harvested from elsewhere in the patient's body. Now, 20% of bone grafts use composite materials based on polymer resins.
The same principle applies to the polymer composites for bone replacement or temporary implants. For many years, broken bones have been mended with metal implants or replaced with bone harvested from elsewhere in the patient's body. Now, 20% of bone grafts use composite materials based on polymer resins.
Their composition can be tailored so that the material degrades as the broken bone heals. This does away with the need to remove the implant once the bone has mended, unlike metal prostheses.
Moreover, recent research has come up with artificial bone made of porous ceramic particle/polymer matrix composites. The patient’s bone cells are injected into this resorbent replacement material and grow within it to reconstruct the missing bone.
True-to-life plastics
Recent research on the polymers used in implant manufacture has led to solutions for reconstructing human body parts or simulating their natural functioning.
The team headed by Didier Letourneur, at the INSERM Laboratory of Cardiovascular Bioengineering in Paris, has succeeded in reconstructing blood vessels from biodegradable polymers. These materials, in the form of tiny tubes, form a 3D matrix on which cells are grown to produce artificial veins or small arteries. The polymer’s porosity allows cells colonise inside the material and when the stent is absorbed, a new vessel has grown inside as if by magic!






